Child And Maternal Malnutrition Continues To Haunt, Indians Falling Prey To Lifestyle Diseases Spikes, Says Health Of India’s States Report
21 Nov 2017 11:16 AM GMT
A recent report titled “India: Health Of The Nation’s States” has brought out the disparity in the country with regards to the challenges in the health sector. This report is based on a study of disease patterns in India from 1990 to 2016. The study was conducted by the Indian Council of Medical Research (ICMR), Public Health Foundation of India (PHFI) and the Institute of Health Metrics and Evaluation.
What is the report
This is the first ever report on the state-level disease burden. It reported that some states that are placed higher on the development ladder are not better than others regarding health. The study further shows that states in the government’s Empowered Action Group (EAG) – UP, MP, Bihar, Rajasthan, Jharkhand, Chhattisgarh, Odisha and Uttarakhand, continue to battle with child and maternal malnutrition. Each state has its own set of health stories to deal with as the limitations to tackle the situation are unique to each state. This shared responsibility explains the massive health inequality among states.
The report “India: Health of the Nation States India State-Level Disease Burden Initiative” was released by Vice President of India Venkaiah Naidu and its findings have been summed up in The Lancet.
This massive report has studied 333 disease conditions, injuries and 84 risk factors across 30 states over 26 years. It also enshrines policy suggestions about each state and has specific chapters. In this report, disease and risk have been analysed at a great level of granularity, and it has been composed into a single comprehensive document. It examines India’s health in a postcolonial framework and seeks an answer to the question that should health remain a state subject in the country?
Health is one of the sectors in India where the centre allocates fund for each state, and specific policy-making and legislation is also done at the central level. But, the states have a much broader scope in implementing all of these as well as doing something more than what the Centre prescribes. The report points out how the health scenario functions uniquely in each sub-national level.
Areas of problem and metrics to measure
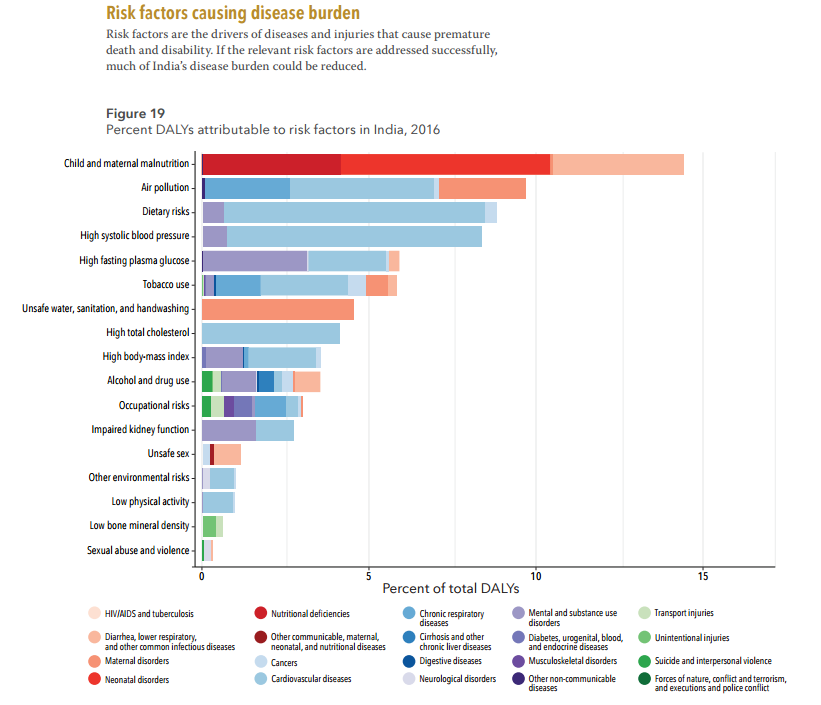
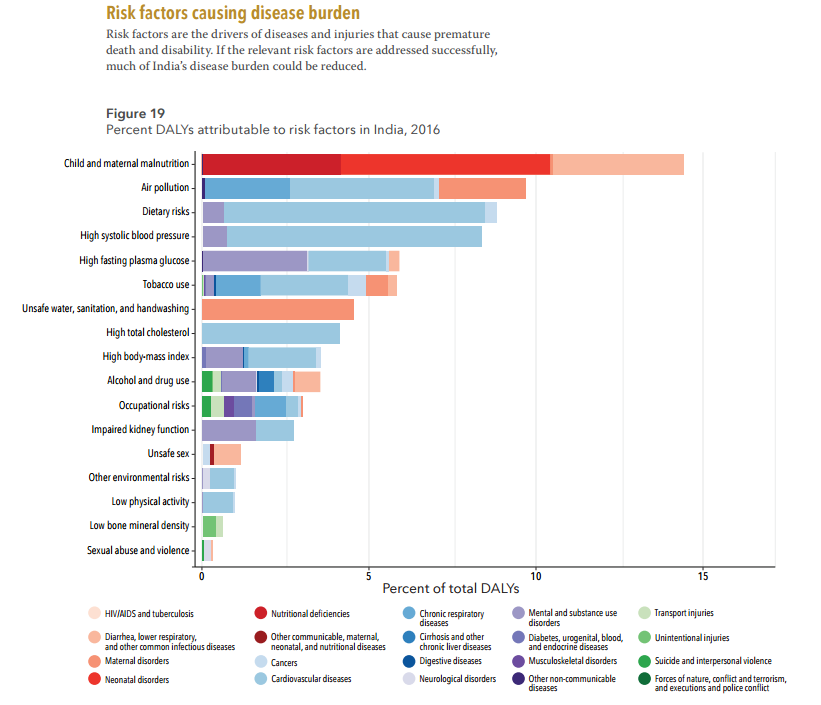
To reach the findings, one common and internationally recognised metric to rate a disease or health condition is DALY (Disability Adjusted Life Years) and is calculated as the sum of years of life due to premature mortality and the years lost due to people living with a health condition or suffering its consequences. A higher DALY metric refers to severe disease burden.
The ‘India State-level Disease Burden Initiative’ compares the health of citizens in 2016 with that in 1990. This report upturns the wide perception that states performing well in economic yardsticks are also performing well in the health sector.
While analysing the report card, let’s take a look at the good news first:
- Life expectancy has shot up by over 10 years: up from 59.7 years in 1990 to 70.3 years in 2016. Women here have an edge over men.
- Socio-economic development of the country is in tandem with the communicable diseases. Traditionally, communicable diseases have been a bane for us.
- This is a drop in the number of incidences of malnutrition, diarrhoea, anaemia and tuberculosis in states like Punjab, Tamil Nadu and Kerala.
- Infant mortality rates show signs of improvement and immunisation rates also shows a sharp rise.
- Mortality due to communicable, maternal, neonatal and nutritional diseases (CMNNDs) declined from 61% in 1990 to 33% in 2016.
- Kerala and Goa show the lowest rate of disease burden.
Now, let us take a look at the areas which are problematic:
- States like Tamil Nadu, Kerala, Goa and Punjab have become hubs of non-communicable diseases (NCDs) including cancer and lifestyle-linked diseases like heart ailments and diabetes.
- Bihar and UP are still battling diarrhoea deaths in children.
- For Chronic Obstructive Pulmonary Disease (COPD), the highest DALY rates were in Rajasthan, Uttarakhand, Uttar Pradesh followed by Himachal Pradesh, Haryana and Jammu Kashmir.
- Malnutrition and communicable diseases continue to perturb states like Jharkhand, Uttar Pradesh, Madhya Pradesh, Chhatisgarh, Uttarakhand and Odisha.
- DALY rates for heart strokes was highest in West Bengal, closely followed by Odisha, Tripura, Assam and Chhatisgarh.
- Lower respiratory infections were highest in Rajasthan, Bihar, UP, MP and Assam.
- TB is highest in UP, followed by Assam, Gujarat, Rajasthan, Odisha and Chhattisgarh
- Disease profile varies across states. NCDs accounted for 37.9% deaths in 1990 and 61.8% in 2016.
- In the North East, Tripura saw 159% higher cases of iron-deficiency anaemia as compared to its neighbour Manipur.
- Manipur has higher incidents of TB, road injuries and neonatal disorders.
- UP, Assam and Chhatisgarh have reported the highest rates of disease burden.
- The share of NCDs in total burden of diseases have increased to 55% from 30% in these 26 years
- Though Kerala has the lowest disease burden in the country, it is 2.7% higher than per person in China


Malnutrition continues to haunt us
The Public Health Foundation of India, Institute for Health Metrics and Evaluation says that malnutrition caused maximum death and disability in 1990 and it is maintaining its position till now in 2016. This still remains to be the single largest risk factor responsible for 15% of the total disease burden. The report said, “This burden is higher in females than in males. Child and maternal malnutrition in India were 12 times higher per person than in China in 2016.” In Gujarat, as many as 10.6% deaths in 2016 were in the age group of 0-14. Maharashtra stands at 6% and Orissa at 9% in terms of deaths in the age group of 0-14 years.
In 1990, malnutrition caused 36.1% death and disability, while in 2016, it caused 14.6% death and disability, the report says. On the other hand, 10.4% death and disability in 2016 were caused due to dietary risk while, 9.1% death and disability were a result of air pollution.
The study also reveals that there is a high percentage of deaths among children in the age group of 0-14 in 2016. Gujarat stands at number 6 in the index. In a report by The Indian Express Dr Leela Visaria, honorary professor at the Gujarat Institute of Development Research said, “This is a very telling tale of the health status of children. It also, in a sense reflects the nutritional status of mothers when low birth-weight babies are born whose chances of survival are greatly compromised.”
Health Commissioner Dr Jayanti Ravi said, “We want to make sure that the existing programmes to deal with malnutrition are targeted in places where we see a lot of cases.”
Risk of cardiovascular diseases
One of the major highlights of the report is the increased risk of cardiovascular diseases. The report shows an increase in the incidence of diabetes and ischaemic heart diseases between 1990 and 2016 by 174% and 106% respectively. The risk of Indians falling prey to lifestyle disease was highest in Punjab, Tamil Nadu, Kerala, Andhra Pradesh and Maharashtra in 2016. The contribution of these risks has increased in every state of the country since 1990. This means India needs a more targeted health policy to resolve the issues.
The report also informs that unsafe water and sanitation was the second leading risk in 1990 but dropped to seventh in 2016 contributing to 5% of the total disease burden. “The per person disease burden due to unsafe water and sanitation was 40 times higher in India than in China in 2016,” the report says focussing on the potential of the current government’s Swachh Bharat Abhiyan.
Outdoor and indoor pollution is another problematic area as pointed out by the report. The report points out that outdoor air pollution was responsible for 6% of total disease burden in India in 2016. This comes at a time when thick grey smog hangs heavily over the national capital and the entire NCR region.
Poverty is a common determinant of all types of diseases. Most diseases can be tackled through improvement in living conditions such as a better supply of drinking water, sanitation facilities, better housing and reduction of outdoor and indoor pollutants etc. We have the knowledge to address the ‘diseases of poverty’ (a common name for CMNDDs) but the knowledge is unevenly dispersed. Knowledge regarding vaccination, antibiotics, nutrition, safe water supply and sanitation have been available for decades. Yet the fact that millions still die from infectious diseases, undernutrition and birth-related conditions is a mirror to the persistent inequality within the country.
The report states, “India’s states will require very different policy approaches according to the nature of the disease burden they are facing.” This calls for more decentralised health planning which has been echoed by both, NITI Aayog Action Agenda 2017-2020 and the National Health Policy 2017.
In a report by The Indian Express Dr Soumya Swaminathan, deputy director-general for programme WHO and former director-general, Indian Council of Medical Research (ICMR) said, “The NCD burden is high in the southern states and in Punjab. Lifestyle is a factor. But it is possible that because for years, especially since the National Rural Health Mission was started in 2005, the focus of primary health centres and sub-centres has been on reproductive and child health because infant and maternal mortality rates were among the MDGs (Millennium Development Goals). So they have been focussing on prevention or spreading awareness about dietary requirements. That is why the National Health Policy talks about shifting towards tackling the NCDs.”
Also read,
India Worst In The World For The Highest Number Of People Without Basic Sanitation
 All section
All section